Regulation of energy balance
Learning outcome 1: To explain the role of hypothalamus in energy balance
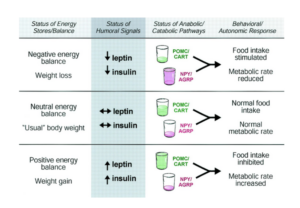
The hypothalamus plays a crucial role in maintaining energy balance in the body by regulating hunger and metabolism. It receives signals from hormones and other parts of the body about the body’s energy status and accordingly stimulates or suppresses hunger and metabolism. For example, when energy stores are low, the hypothalamus stimulates hunger and reduces metabolism, and when energy stores are high, it suppresses hunger and increases metabolism.
The arcuate nucleus, located in the hypothalamus, plays a central role in the regulation of energy balance. The arcuate nucleus contains two populations of neurons that have opposing effects on hunger and metabolism.
- The hypothalamic-pituitary-adrenal (HPA) axis: This pathway is activated when energy stores are low, and it stimulates hunger and reduces metabolism. The HPA axis releases corticotropin-releasing hormone (CRH) and arginine vasopressin (AVP), which stimulate the release of cortisol and adrenocorticotropic hormone (ACTH) from the adrenal glands. Cortisol and ACTH then increase hunger and reduce metabolism.
- The melanocortin pathway: This pathway is activated when energy stores are high, and it suppresses hunger and increases metabolism. Neurons in the arcuate nucleus release pro-opiomelanocortin (POMC) and cocaine- and amphetamine-regulated transcript (CART), which stimulate the release of melanocortins, such as alpha-melanocyte-stimulating hormone (α-MSH), from the hypothalamus. α-MSH then suppresses hunger and increases metabolism.
Both the HPA axis and the melanocortin pathway are regulated by hormones and other signals related to energy balance, such as insulin and leptin, which are produced by adipose tissue, and ghrelin, which is produced by the stomach. These hormones and signals act on the arcuate nucleus to stimulate or suppress hunger and metabolism, depending on the body’s energy status.
In conclusion, the arcuate nucleus plays a key role in the regulation of energy balance by integrating signals related to energy balance and controlling hunger and metabolism through the HPA axis and the melanocortin pathway.
This diagram below summarises the relationship between energy balance, humoral signals and anabolic/catabolic pathways.
Learning outcome 2: To describe the role of gut hormones and adipose tissue in the regulation of energy balance
The regulation of energy balance is a complex process that involves multiple hormones and tissues in the body.
Gut hormones play a crucial role in the regulation of energy balance by signaling to the brain about the presence of food in the digestive system. They are released in response to food intake and can increase or decrease hunger and metabolism. For example, cholecystokinin and glucagon-like peptide-1 (GLP-1) increase feelings of fullness and slow down digestion, while ghrelin stimulates hunger and speeds up digestion.
Adipose tissue, also known as body fat, also plays a role in regulating energy balance by releasing hormones known as adipokines. Adipokines, such as leptin and adiponectin, signal to the brain about the amount of fat stored in the body and influence hunger, metabolism, and energy expenditure. For example, high levels of leptin signal that energy stores are adequate, leading to decreased hunger and increased metabolism, while low levels of leptin signal low energy stores, leading to increased hunger and decreased metabolism.
White adipose tissue ‘the WAT’:
- White adipose tissue (WAT) is one of the two main types of body fat, the other being brown adipose tissue. It is widely distributed throughout the body and serves as a primary energy storage site for excess caloric intake.
- WAT is composed of mature adipocytes, which are specialized cells that store fat in the form of triglycerides. These triglycerides are stored in large lipid droplets within the adipocyte, making WAT appear white in color.
- WAT has several important functions in the body, including insulation, cushioning, and releasing hormones that regulate hunger and metabolism. For example, leptin, an adipokine produced by WAT, signals to the brain about the amount of fat stored in the body and influences hunger, metabolism, and energy expenditure.
- However, when the body accumulates excessive amounts of WAT, it can lead to obesity and increase the risk of associated health problems, such as type 2 diabetes, heart disease, and certain types of cancer.
In conclusion, white adipose tissue is a crucial component of the body’s energy balance system and plays important roles in the regulation of hunger and metabolism. However, excessive accumulation of WAT can have negative health consequences.
Learning outcome 3: To discuss the consequences of dysregulation of energy balance.
Dysregulation in adipokine secretion:
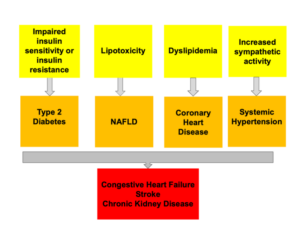
Dysregulation of energy balance, or the failure of the body to properly regulate hunger and metabolism, can have serious health consequences. Some of the most common consequences include:
Dysregulated adipokine secretion refers to an abnormal or imbalanced release of signaling molecules called adipokines from fat (adipose) tissue. Adipokines play a crucial role in regulating metabolism, immune function, and inflammation. This leads to an accumulation of free fatty acids.
The effects of free fatty acids in plasma:
Free fatty acids (FFAs) in plasma have several effects on the body, including:
- Insulin resistance: High levels of FFAs in the bloodstream can impair insulin sensitivity and increase the risk of type 2 diabetes.
- Lipotoxicity: Excessive FFAs can accumulate in liver and muscle tissues, leading to cellular damage and inflammation, a condition known as lipotoxicity.
- Inflammation: FFAs can stimulate the release of pro-inflammatory cytokines, which can contribute to the development of chronic diseases such as obesity, cardiovascular disease, and type 2 diabetes.
- Increased oxidative stress: FFAs can increase the production of reactive oxygen species (ROS), which can cause oxidative damage to cells and tissues.
- Cardiac dysfunction: Elevated FFAs levels in plasma have been linked to impaired cardiac function and increased risk of heart disease
Carbohydrate metabolism:
Carbohydrate metabolism refers to the process by which the body converts carbohydrates into energy. The process of carbohydrate metabolism can be divided into several stages, including:
- Digestion: Carbohydrates are broken down into smaller units, such as glucose, in the small intestine through the action of digestive enzymes
- Absorption: Simple sugars like glucose are absorbed into the bloodstream and transported to cells.
- Glycolysis: Glucose is converted into pyruvate, which releases energy and produces ATP (adenosine triphosphate) in a process called glycolysis.
- Krebs cycle: Pyruvate enters the mitochondria, where it is converted into acetyl-CoA and enters the Krebs cycle (also known as the citric acid cycle). This cycle produces more ATP and generates the precursors for biosynthesis.
- Oxidative phosphorylation: In the final stage of carbohydrate metabolism, the electrons generated in the Krebs cycle are used to generate ATP through oxidative phosphorylation.
The rate of carbohydrate metabolism is influenced by various factors, including the availability of glucose, the demand for energy, and hormones such as insulin and glucagon. Abnormalities in carbohydrate metabolism, such as those seen in type 1 and type 2 diabetes, can lead to serious health problems.
Lipid metabolism:
Lipid metabolism refers to the process by which the body converts lipids (fats) into energy. The process of lipid metabolism can be divided into several stages, including:
- Lipolysis: Lipids are broken down into smaller units, such as fatty acids, by the action of lipases, enzymes that break down fats.
- Transport: Free fatty acids are transported in the bloodstream bound to albumin, a protein, to the cells that need energy.
- Beta-oxidation: In the cells, fatty acids are converted into acetyl-CoA, which enters the Krebs cycle (also known as the citric acid cycle) and releases energy. This process is called beta-oxidation.
- Ketogenesis: When glucose is not available, the liver converts fatty acids into ketone bodies, which can be used as an energy source by the brain and other tissues.
- Lipogenesis: Lipogenesis is the process of converting excess glucose into fat for storage in adipose tissue.
The rate of lipid metabolism is influenced by various factors, including the availability of glucose, insulin levels, and the demand for energy. Abnormalities in lipid metabolism, such as those seen in conditions such as hyperlipidemia and fatty liver disease, can lead to serious health problems.
Consequences of obesity: